The Body Dysmorphic Disorder Questionnaire – Aesthetic Surgery (BDDQ-AS) is a brief screening tool developed for cosmetic settings where a practitioner may wish to screen a patient for body dysmorphic disorder (BDD).
The BDDQ-AS includes 7 items which assess the core dimensions of BDD, namely preoccupation with flaws in physical appearance, appearance-related distress and interference with social, occupational or role functioning.
The BDDQ-AS is designed as a screening tool, rather than a diagnostic tool, and is not considered to be an official diagnosis of BDD. An official diagnosis should be made by a suitably qualified mental health professional.
There is strong empirical and theoretical basis indicating that the presence of BDD poses a psychological risk for patients undergoing cosmetic procedures (Honigman et al., 2004; Moulton et al., 2018, Pikoos et al., 2021). For example, 82.3% of individuals with BDD who undergo cosmetic procedures will experience no improvement or worsening in their mental health condition after the procedure, and many report dissatisfaction with the outcomes (Bowyer et al., 2016). Individuals with BDD are at three times higher risk of experiencing complications and more significant post-operative pain, when compared to a control group (Wooley & Perry, 2015).
The Medical Board of Australia guidelines (2023) stipulate that cosmetic practitioners should screen for BDD using a validated assessment tool, prior to administering any cosmetic surgery or non-surgical procedures. The BDDQ-AS is a validated screening measure which is fit for this purpose (Lekakis et al., 2016).
A patient screens positive for BDD if they acknowledge on the BDDQ-AS that they are concerned about their appearance (question 1 = yes) AND preoccupied with these concerns (question 2 = yes) AND that these concerns cause at least moderate distress or impairment in different domains of daily life (any of question 3 or 4 or 5 or 6 ≥ 3 or question 7 = yes).
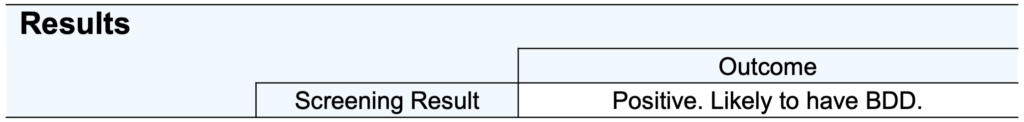
The BDDQ-AS is a screening tool, and is therefore not designed to provide a diagnosis of body dysmorphic disorder (BDD). Patients who screen positive on the BDDQ-AS should be referred to a mental health professional for further assessment.
The BDDQ-AS is a seven-item questionnaire validated in 116 patients undergoing aesthetic rhinoplasty. It was an adapted version of the Body Dysmorphic Disorder Questionnaire – Dermatology Version (Dufresne et al., 2001), with the goal of making it less time-consuming and easier for the aesthetic practitioner to score.
In the validation sample, the BDDQ-AS had a Cronbach alpha of .83, and .84 for controls, indicating high internal consistency. Test-retest reliability over a one-month period was satisfactory (rho = 0.86). 47% of people scored positive on the BDDQ-AS, with those screening positive also scored highly on related measures such as the Sheehan Disability Scale and the Derriford Appearance Scale. When compared to the gold standard measure of BDD symptoms, the Yale Brown Obsessive Compulsive Scale – BDD version (BDD-YBOCS), the BDDQ-AS had 89.6% sensitivity and 81.4% specificity. The BDDQ-AS has also been associated with lower postoperative satisfaction at 12 months following rhinoplasty surgery, indicating it’s predictive utility.
Since it’s development, the BDDQ-AS has been implemented widely across several other research studies.
The high proportion of people scoring above the BDD cut-off is not uncommon in populations seeking cosmetic procedures (Veale et al., 2016; Lekakis et al., 2016). For a more nuanced decision-making process regarding the risk profile of patients screening positive for BDD, we recommend administering the Cosmetic Readiness Questionnaire (CRQ).
Developer
Lekakis, G., Picavet, V. A., Gabriëls, L., Grietens, J., & Hellings, P. W. (2016). Body dysmorphic disorder in aesthetic rhinoplasty: validating a new screening tool. The Laryngoscope, 126(8), 1739-1745.
References
Bowyer, L., Krebs, G., Mataix-Cols, D., Veale, D., & Monzani, B. (2016). A critical review of cosmetic treatment outcomes in body dysmorphic disorder. Body Image, 19, 1-8.
Dufresne Jr, R. G., Phillips, K. A., Vittorio, C. C., & Wilkel, C. S. (2001). A screening questionnaire for body dysmorphic disorder in a cosmetic dermatologic surgery practice. Dermatologic Surgery, 27(5), 457-462.
Honigman, R. J., Phillips, K. A., & Castle, D. J. (2004). A review of psychosocial outcomes for patients seeking cosmetic surgery. Plastic and reconstructive surgery, 113(4), 1229.
Lekakis, G., Picavet, V.A., Gabriëls, L., Grietens, J. and Hellings, P.W. (2016), Body Dysmorphic Disorder in aesthetic rhinoplasty: Validating a new screening tool. The Laryngoscope, 126: 1739-1745. https://doi.org/10.1002/lary.25963
Moulton, S. J., Gullyas, C., Hogg, F. J., & Power, K. G. (2018). Psychosocial predictors of body image dissatisfaction in patients referred for NHS aesthetic surgery. Journal of Plastic, Reconstructive & Aesthetic Surgery, 71(2), 149-154.
Pikoos, T. D., Rossell, S. L., Tzimas, N., & Buzwell, S. (2021). Is the needle as risky as the knife? The prevalence and risks of body dysmorphic disorder in women undertaking minor cosmetic procedures. Australian & New Zealand Journal of Psychiatry, 55(12), 1191-1201.
Veale, D., Gledhill, L. J., Christodoulou, P., & Hodsoll, J. (2016). Body dysmorphic disorder in different settings: A systematic review and estimated weighted prevalence. Body Image, 18, 168-186.
Woolley, A. J., & Perry, J. D. (2015). Body dysmorphic disorder: prevalence and outcomes in an oculofacial plastic surgery practice. American Journal of Ophthalmology, 159(6), 1058-1064.